As living organisms, bacteria are encoded by DNA, and DNA occasionally mutates. Sometimes genetic mutations render a bacterium immune to an antibiotic’s chemical tactics. The few cells that might escape antibiotic pressure then have a sudden advantage: with their counterparts wiped out, resources abound, and the remaining antibiotic-resistant bacteria proliferate. It’s a problem not only for the host—you or me when we are treated with an antibiotic and develop a resistant strain—but also for anyone with whom we happen to share our resistant bacteria, say, on a door handle or keyboard. In fact, most resistant bacteria develop not in people but in livestock fed antibiotics to promote growth; these resistant bacteria infect people through contaminated animal products. This is how even antibiotic “naive” people come to be infected with resistant strains of bacteria.
I see this all the time as a family doctor. A woman has a urinary tract infection. I tell her that her bacteria are resistant to this or that antibiotic, and she says, “But I’ve never taken any of those.” Welcome to the global human soup.
We should have stopped irresponsible use of antibiotics decades ago.
But capitalism decided.
Did the USSR not use antibiotics or something?
From the article …
WHILE PHAGE THERAPY was largely abandoned after the 1940s during the so-called golden age of antibiotics, microbiologists in Eastern Europe and former Soviet republics continued using phages in research and clinical applications.
Sure but they still used antibiotics and had their own production lines.
One of my professors in university was a leading researcher in bacteriophage therapy. They did some amazing things in the 2000s with them, like elimination of only pathogenic strains of E. coli in livestock. I can only imagine what they could do with a budget more inline with pharmaceutical research than that available at a small state school that most students didn’t know had a sciences department.
Australia what are you doing? https://ourworldindata.org/grapher/antibiotic-usage-in-livestock
I don’t trust these figures at all. The USA’s factory farming is gargantuan. Canada is similar to Australia. The only way I could see this chart making sense is if there were diminishing returns in antibiotics at a certain scale or density, which doesn’t sound right either, or the winter climate reduced the need for antibiotics.
It’s impossible to know exactly what we don’t know. This is a big issue, but there are people taking it seriously. It seems likely new antibiotics which will work are going to be developed. For example: this new class that was discovered a couple months ago using AI.
The article discusses the ‘newest’ form of treatment …
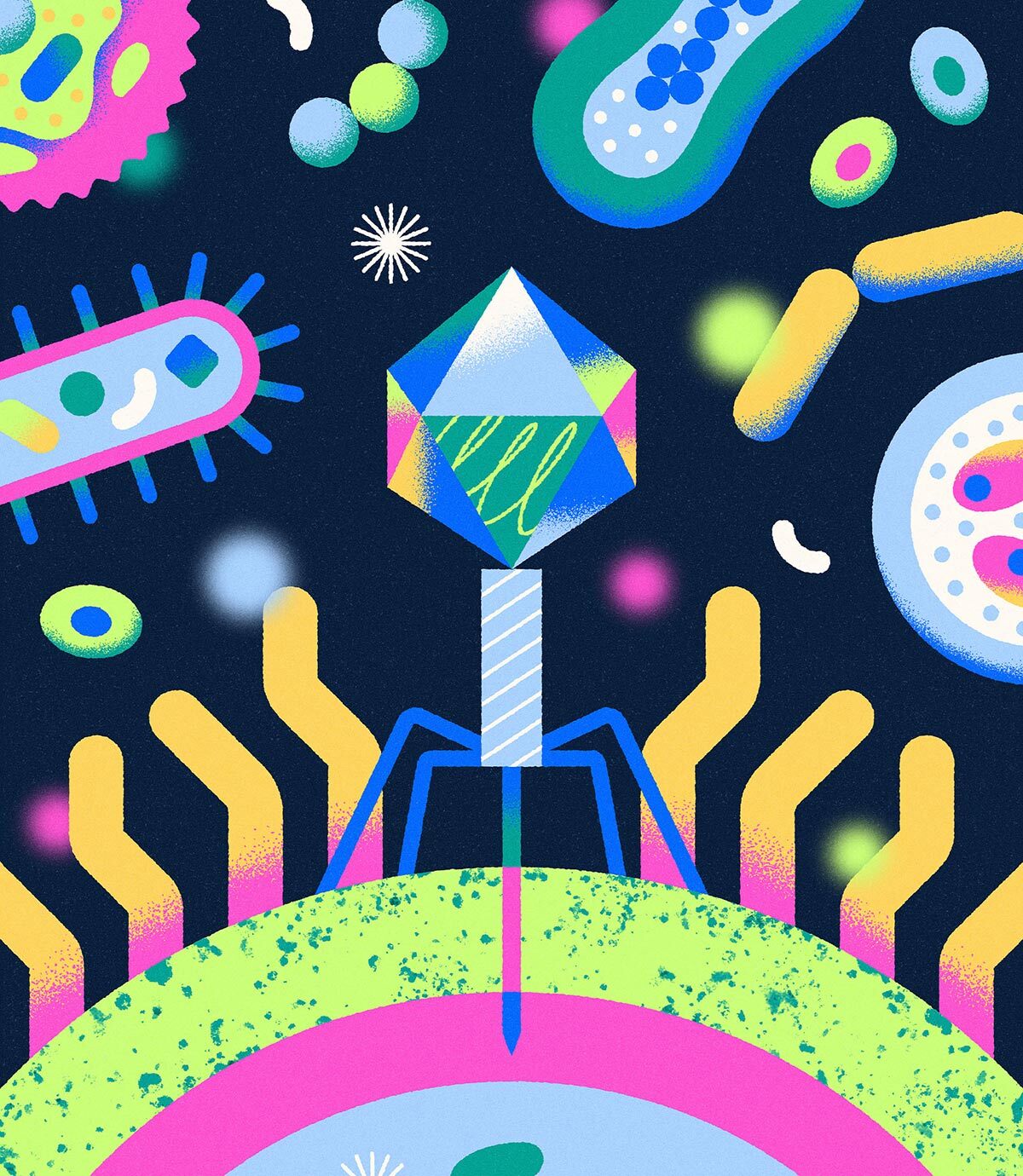
BACTERIOPHAGES, or phages for short, are viruses that attack bacteria and kill them; the two organisms have been involved in an evolutionary cat-and-mouse game for millions of years. Phages are ever present in the environment, from sea water to barnyard waste—anywhere bacteria are found in high numbers.
Phage therapy has issues. It’s generally hyperspecific, with every strain of bacteria having its own phage, most of which we don’t have, and which they can become resistant to.
The article deals with that.
Greg German, a medical microbiologist at Unity Health Toronto, has collaborated at times with Nancy Tawil, a biomedical engineer with experience in phage production for the US-based company Precisio Biotix Therapeutics and as CEO of Qeen BioTherapeutics based in Gatineau, Quebec. For years, her production teams have been collecting libraries of phages from all over the world that infect and kill common human pathogens, such as Staphylococcus, Pseudomonas, Klebsiella, and Acinetobacter, all of which can cause life-threatening lung, brain, and blood infections. To date, most of Tawil’s research has been done on patients in the US. Qeen receives a sample of infected tissue, isolates the bacteria, screens its library for an effective phage—usually a cocktail of up to five phages—then ferments, multiplies, and purifies the phages, and delivers the mixture to the clinical team. That process takes between a week and two weeks. The price tag? About $45,000. According to Tawil, that’s the cost of making 200 litres of phage solution, whereas a patient might need only fifty millilitres for their treatment. Sometimes a phage found for one person can also work on another, reducing the cost of treatment per person.
oh, great
You can’t cheat evolution.
People often cite evolution for antibiotic resistance, but that’s not the case.
There’s an inverse relation between bacteriophage resistance and antibiotic resistance. Antibiotic resistance requires more efflux pumps and less strong cell walls, and bacteriophage resistance requires stronger cell walls and less efflux pumps.
What’s happening is allele drift within colonies towards better antibiotic resistance, but these colonies are also very susceptible to bacteriophages.
This is no different than the frequency of spots on deer in a population group increasing our decreasing over generations.
I know many people call that evolution, but I think it’s important to be precise with our definitions. These traits for antibiotic or bacteriophage resistance are already present within the genome. They each just get expressed under different conditions, and the phenotypic strength of each is inversely proportional to the expression of the other.
This isn’t a simple or straightforward relationship. Genetics are always incredibly complex, but this relationship is confirmed.
I understand what you’re saying about drift, but I’m not sure that feels sufficient to explain the prevalence of anti-biotic resistance. You’re right to highlight that the genes for antibiotic resistance already exist and it’s just a question of how prevalent they are in different populations/generations, but I don’t think this excludes it from being evolution. I would consider the human use of antibiotics in medicine and agriculture to be a selective pressure that is increasing the prevalence of antibiotic resistant genes in bacteria, especially in combination with human activities that facilitate the global spread of antimicrobial resistance.
I agree that “evolution” is a pretty muddy term though, which is made trickier by the fact that with how language evolves, some people use it in a different sense than what is probably strictly “correct”. I’m a biochemist, for example, and I don’t know if I could give a strictly correct definition for evolution. Along those lines, I realise I may be misinterpreting your point.
Separate to all that, it sounds like you’re well versed on the bacteriophage stuff, are there any articles that you think cover the topic well? I’m more of a protein structure gal myself, so I only have patchy, undergrad level knowledge of microbiology stuff.
I understand what you’re saying about drift, but I’m not sure that feels sufficient to explain the prevalence of anti-biotic resistance.
One interesting discovery was the remains of a person in Peru from something like 900 years ago. One really interesting aspect of the discovery was the gut bacteria in the remains. When they sequenced the genome of some of the bacteria they found that they were the same species as we have today. But more importantly was that the genes that encode for antibiotic resistance existed in those bacteria.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4589460/
The discussion here isn’t about how antibiotic resistance first came about, the discussion is about how bacteria have been reacting to modern medicine. Why are bacteria becoming harder to treat with antibiotics as time goes on?
The point I was making is that bacteria already have antibiotic resistance in the genome, but the phenotypic expression is inversely related to bacteriophage resistance.
Antibiotic resistance needs
-
weaker/more flexible cell walls
-
more efflux pumps
Bacteriophage resistance needs
- stronger/stiffer cell walls (to protect against punctures)
- less efflux pumps (to increase material strength of cell wall)
In any population group there’s going to be variation in the expression of genes (the phenotype). In that population there are going to be individuals with greater antibiotic resistance and others with greater bacteriophage resistance. When antibiotics are introduced it kills most of the bacteria, but there can be a few individuals with higher antibiotic resistance that can potentially repopulate a new generation with an allele frequency shifted towards higher antibiotic resistance.
I know what I just described is “natural selection”, but that’s not evolution. Natural selection is one of the processes that is part of evolution, but it is not evolution in of itself.
Edit: formatting
-
A succinct definition of evolution is “The change of allele frequencies over time.” Even “allelic drift” is evolution.
For bacteria, population sizes are big enough that simple variants like base substitutions can occur at every single base in the genome over a short period of time. Some of these are important to the development and redevelopment of resistances. Once one allele has spread enough, compensatory mutations can bring about combinations that weren’t seen before.
Antibiotic resistance is definitely an evolved trait, and it’s the reason why multi-resistance and resistance to brand new antibiotics is becoming such a problem.
Your comment is confusing. Yes, genetic drift is evolution, so saying “people cite evolution” and then dismissing it is not a good approach.
Perhaps you mean it isn’t natural selection, but then the trait being under balancing selection (a tradeoff between phage resistance and antibiotic resistance) is still under selection. And the presence of antibiotics shifts the balance heavily in favor of resistance even if that means decreasing resilience in the absence of antibiotics.
You say the traits are already there and just need to be expressed, so perhaps it’s mutation you think is not happening. That’s often the case, but it still took mutation to create the means of resistance to begin with. Some of it is passed around on plasmids, but they the traits had to evolve in the first place. In addition, once resistance becomes dominant, there is enough diversity to select for compensatory mutations that increase the fitness of the resistant bacteria. Things like compensating for cell wall weaknesses or pumps that were initially favored despite their drawbacks.
Yes, genetic drift is evolution
Not “genetic drift”. Although I did forget a critical word. I meant to say “allele frequency drift” which is distinctly different than genetic drift.
Allele frequency drift simply describes a shift in how common a genetic trait exists, or is expressed, within a population group. The overall genetics of the group are the same. Even if there were no changes to the collective genetics of a population over millions of years (no evolution) you can still have allele frequency drift.
This is what I mean by “allele frequency drift isn’t evolution”. It’s a mathematical expression of the ratio a gene is expressed within a population group. It doesn’t describe any genomic changes or mutations.
The first generation can have frequency 1.0 of a trait, gen 2 can have 1.5, gen 3 can have 2.0, and then back down again over the next few generations. But generation 10 can have an (nearly) identical genome to generation 1.
You are reporting one side of a three-sided coin. You can find instances of phage resistance linked to increased antibiotic susceptibility, decreased antibiotic susceptibility, and in most cases no change in antibiotic susceptibility. Studies linking phage resistance to increased antibiotic susceptibility are based on in vitro selections resulting in genetic disruptions that would never arise in a host, and are likely due to the relaxation of selective pressures when bacteria are grown in rich broth. For example, phage that use LPS as a receptor cannot infect cells with LPS defects, but those cells are so sick and mucoid that they become susceptible to just about any other stress, including antibiotics. We never isolate bacteria with LPS defects in the wild because they would go extinct in any competitive environment.
The real lessons we need to learn from phages and other antibacterial systems is that resistance is inevitable. These systems have built in flexibility and modularity to accommodate changes and mutate rapidly. Almost all of these systems follow a similar pattern: bind to target cell, get inside target cell, destroy target cell. There are many ways to accomplish each of those steps, and these systems are set up to rapidly evolve new ways accomplish each. This evolution is not limited to the slow single mutations we often associate with evolution. We often observe recombination where another target cell binding domain can be swapped in to generate a new functional system.
Modern phage therapy advocates suggest combination therapies, where multiple antibacterial agents are deployed to substantially lower the rate of resistance. But we will never get that number to zero. Also phage therapy is limited in efficacy based on the site of infection (phage do not penetrate tissues like small molecule antibiotics do) Instead of evolution being a brick wall for therapy, we need to play the game. We need to get off of broad-spectrum antibiotics, focus on functional modules (like cell entry, cell toxicity, etc), and reform our regulatory structure to enable mixing and matching of these modules in regimented phases in response to the resistance that we know will arise. Phage therapy is not the answer; the phage evolutionary cycle is the answer.
Ive nearly shit myself to death over the last 2 weeks thanks to antibiotic resistant campylobacter. Hoping the 3rd and 4th antibiotics can help me get rid of this thing.
Another reason to become vegetarian.
vegetarians still support the egg and dairy industry, which use massive amounts of antibiotics. the solution is veganism.
I know, but seeing the number of downvotes, it seems that many people still prefer to deny the problems.
A vegetarian that eats eggs is a sith.
Lemmy hates vegetarians. Just look at all the pro meat propaganda posted. They’re not even aware of that yet.
Which is surprising as becoming vegetarian is one of the best things you can do, as an individual, for the climate. It also tends to be quite healthy.
I’m not sure right now: Is my above comment downvoted because I wrote “vegetarian” and not “vegan”? Or are there really so many advocates of meat consumption here?
Given that in the real world there is propaganda to eat meat on every street corner, which is echoed everywhere online, I bet it’s the latter.
What are you talking about? Beans are totally vegetarian…
Another reason to regulate industry, as has already begun in the US and EU. Relying on individual behavioural changes to solve these types of systemic failures simply does not work.
But I’m glad it gives you a reason to feel morally superior.
I see those as complementary. In a democracy, political change can only come when individuals support it. Division is what prevents progress. Try to be decent and excellent.
They’re not.
History has proven over and over again that systemic change doesn’t happen through voluntary individual action unless government creates incentives or nudges to drive that action.
Admonishing people to eat less (or no) meat won’t solve the problem of antibiotic resistance any more than asking them to pollute less fixed global warming.
If anything, asking individuals to sacrifice to solve a problem caused by industry will just harden people against action as it directs blame in exactly the wrong direction.
The dichotomy of individuals and society/government is just an illusion. The government consists of individuals too. And every systemic change that was achieved through legislation is crafted by individuals in the government, who as a group formed new principles. Every single time when a new law is created in a democratic society, there has to be a critical mass of people who bring up that topic.
I don’t know where you live, but am not living in a kingdom or a monarchy where I look up to THE GOVERNMENT as some entity that decides over all the actions of the people, and to which I transfer full responsibility for my live and future.
As responsible people, we should not use the excuse that the system is against us when it comes to everyday life.
And by the way: a vegetarian or vegan or ecologically sensible lifestyle is not a “sacrifice”, but the free decision to lead a healthy and sustainable life. If someone wants that for themselves and their family, then you don’t wait for the government.
That doesn’t mean that I am against regulation of the industry. I simply said, if someone wants to avoid taking antibiotics with food, it’s a good reason to not eat meat.
deleted by creator
The US still allows Bayer to monopolize GMO seeds and herbicide in America, so it ain’t doing all it can do.
And the EU recently allowed Round-Up GMO seeds and herbicide usage … so not that good either.
Monoculture farming probably isn’t helping this either, if anything it makes it worse as a blight affecting a specific plant now hits harder. The US learned absolutely nothing from the dust bowl and has entire states full of corn and cows.
I’d rather they don’t. As long as others are dependent on meat, their total fitness shall remain lower than mine, giving me a very real competitive advantage.